
Some people eat carefully, watch portions, and still see weight gain. The scale creeps up slowly, energy feels low, and progress feels stuck. It’s confusing-especially when food choices haven’t changed much.
This is where chronic inflammation and body weight become part of the conversation.
After 30, many adults notice fatigue, stiffness, and slower fat loss. Cutting calories harder doesn’t always help. In fact, it can make things worse. One reason is that inflammation often works quietly in the background, affecting how the body responds to food, movement, and stress.
Inflammation isn’t always obvious. There’s no sharp pain or clear warning sign. But over time, it can influence hormones, energy levels, and how easily the body stores fat. That’s why focusing only on calories can miss a bigger issue.
Understanding inflammation doesn’t mean blaming the body. It means learning what’s actually getting in the way of balance.
The Biological and Lifestyle Reasons Inflammation Affects Body Weight
Inflammation is part of the immune system. In simple terms, it’s how the body reacts to a problem, like an injury or infection. Acute inflammation is short-term and helpful. It protects and heals.
Problems start when inflammation becomes low-grade and sticks around.
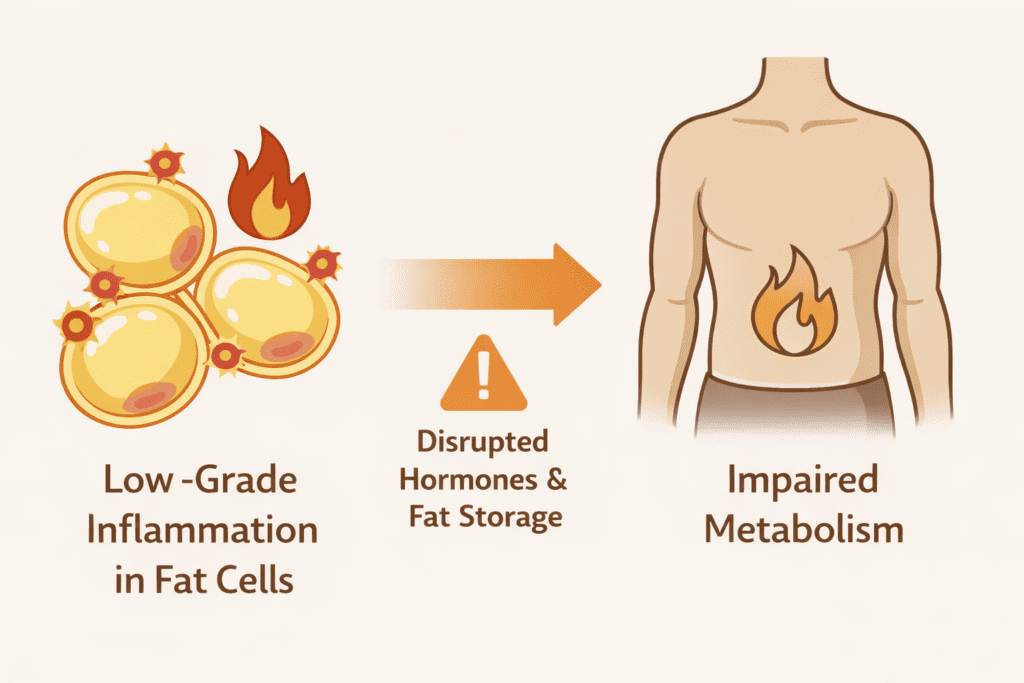
This ongoing inflammatory state changes how the body works. Hormone signals become less clear. Appetite regulation shifts. Fat cells start behaving differently. Over time, this can affect metabolism and lead to excess weight without obvious overeating.
Lifestyle plays a big role. High stress, poor sleep, and frequent intake of processed foods all raise inflammatory signals. A sedentary lifestyle adds to the load. These factors are more common after 30, which is why inflammation-related weight struggles increase with age.
Inflammation may also affect how fat is stored. Adipose tissue can release inflammatory compounds that attract immune cells, creating a feedback loop. This is one reason inflammation and weight are closely connected in conditions like obesity.
The result isn’t sudden weight gain-it’s gradual. Energy drops. Recovery slows. And losing fat becomes harder than it used to be.
How Chronic Inflammation Influences Body Weight
Inflammation doesn’t just affect how you feel. It changes how the body handles energy.
When chronic inflammation is present, hormone signaling becomes less efficient. One key issue is insulin resistance. When cells stop responding well to insulin, glucose stays in the bloodstream longer. This can lead to insulin resistance, which makes it easier for the body to store energy as fat instead of using it.
This process directly connects inflammation and weight gain.
Inflammatory signals can also affect how fat cells behave. Instead of releasing energy when needed, these cells tend to hold on to it. Over time, this encourages fat accumulation, even when food intake hasn’t increased much.
Another overlooked factor is energy. Chronic inflammatory activity increases fatigue. When energy drops, activity levels usually drop too. Less movement means fewer calories burned, which contributes to gradual weight gain.
Recovery also slows down. Muscles take longer to heal, joints feel stiff, and motivation fades. This makes exercise feel harder to maintain. When recovery suffers, the body’s metabolic response weakens, which further slows progress.
This is why many adults struggle to lose weight even when they’re doing “everything right.” Inflammation interferes with normal signals that support fat loss and balance.
Reduced Energy, Fat Storage, and the Vicious Cycle
Here’s where things often spiral.
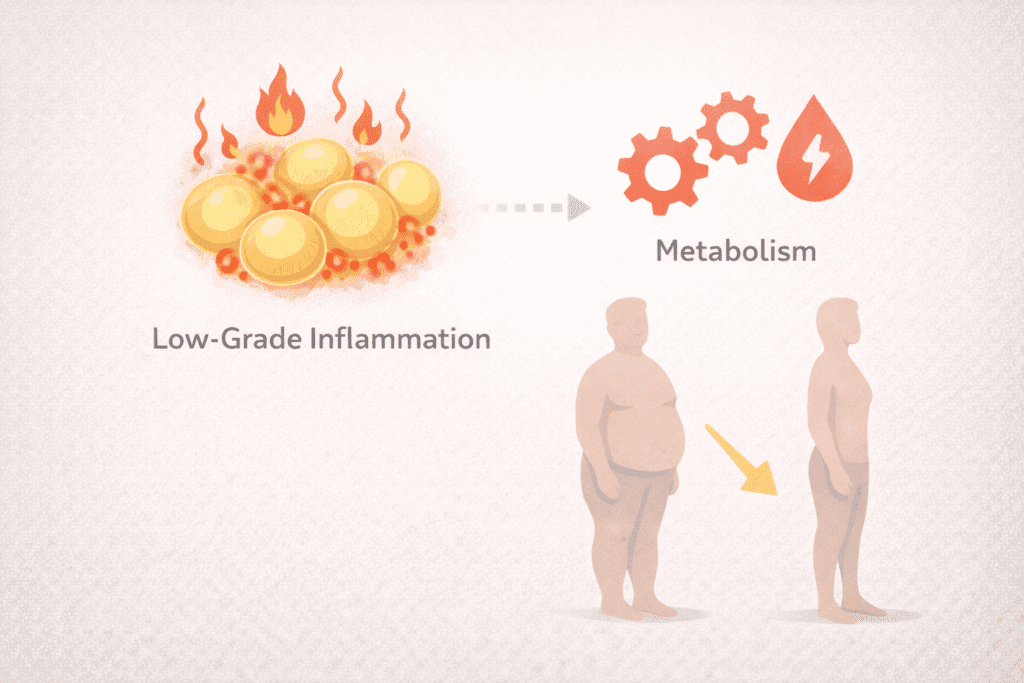
Inflammation affects fat tissue, especially around the abdomen. This tissue releases more inflammatory markers, which then worsen insulin resistance and increase fat storage. The body ends up in a vicious cycle-more inflammation leads to more fat storage, and more fat tissue feeds inflammation.
This cycle is common in metabolic inflammation, where weight, stress, and blood sugar issues overlap. Over time, this pattern increases the risk of conditions like type 2 diabetes, especially when paired with poor sleep and stress.
Inflammation also affects hormones like leptin, which helps regulate appetite. When leptin signaling is disrupted, hunger cues become unreliable. People may eat more without realizing it, or feel unsatisfied after meals.
None of this means weight is out of control. It means the body needs support, not punishment. Addressing inflammation helps restore signals that allow energy to be used properly again.
This is why weight management works better when lifestyle factors-sleep, stress, movement, and food quality-are addressed together, not in isolation.
Stress, Cortisol, and Inflammatory Load
Stress is one of the most underestimated drivers of inflammation.
When stress becomes constant, the body releases more cortisol. In short bursts, cortisol is useful. But when it stays elevated, it increases inflammatory activity and encourages the body to store energy. Over time, this pattern leads to weight gain, especially around the midsection.
Chronic stress also affects how the body processes glucose. Cortisol can push blood sugar higher, which then leads to higher glucose levels and worsens insulin resistance. This creates a situation where the body prefers fat storage over fat use.
This stress-driven inflammatory load becomes more common after 30, when sleep quality drops and responsibilities increase. The body stays in a constant “alert” mode, which makes fat loss harder and recovery slower.
Some people explore supportive options like Nagano Tonic when learning about stress and cortisol balance. It’s usually mentioned in the context of inflammation and support, not as a solution on its own. A detailed review helps readers understand how it fits into a broader lifestyle approach.
The main point here is simple: lowering stress helps calm inflammation. When cortisol settles, the body becomes more responsive again.
Cellular Energy, Mitochondria, and Inflammation
Inflammation doesn’t just affect hormones-it affects energy at the cellular level.
Inside cells, mitochondria are responsible for producing energy. When inflammation stays high, these energy systems experience stress. This reduces output and leads to fatigue. When energy drops, activity drops, and weight gain becomes more likely.
This is where inflammation interferes with progress. Even light movement can feel exhausting. Over time, this reduces calorie use and weakens the body’s ability to burn fat efficiently.
Some people discuss Mitolyn in conversations around cellular energy and mitochondrial support. It’s generally framed as complementary, not essential. Readers usually review it carefully before deciding whether it fits their needs.
When inflammation is addressed, energy production improves. That doesn’t mean instant results-but it does mean the body becomes more capable of steady movement and recovery.
Blood Sugar Imbalance and Inflammatory Weight Gain

Blood sugar and inflammation are closely linked.
Frequent spikes in glucose increase inflammatory responses. Over time, this contributes to insulin resistance, which makes it easier for the body to store fat. This connection explains why weight gain and inflammation often happen together.
Inflammation also affects fat tissue, especially visceral fat. This tissue releases inflammatory compounds that worsen blood sugar control, reinforcing the cycle. The result is gradual weight gain that feels difficult to reverse.
Some people explore Ikaria Lean Belly Juice when learning about blood sugar and insulin balance. It’s usually discussed as part of a supportive routine, not a replacement for dietary changes. Detailed reviews help people decide if it aligns with their goals.
Stabilizing blood sugar helps reduce inflammatory pressure. When glucose levels stay balanced, energy improves and fat storage signals ease.
Morning Thermogenesis and Inflammation
Inflammation doesn’t just affect weight-it affects how active the body feels.
When low-grade inflammation is present, metabolic activity often slows. The body becomes less responsive in the morning, energy feels flat, and movement feels harder to start. This can quietly reduce daily calorie use without people realizing it.
Gentle morning routines can help counter this. Light movement, stretching, or a short walk supports circulation and helps regulate metabolism without adding stress. These habits don’t need to be intense. The goal is to wake the body up, not exhaust it.
Some people mention Java Burn when talking about morning thermogenesis and metabolic balance. It’s usually referenced as part of a routine, not as a fix. Readers interested in it often explore a full review before deciding whether it fits their lifestyle.
The takeaway here is moderation. Supporting metabolic balance in the morning can reduce inflammatory pressure and help the body respond better throughout the day.
Protein Intake, Muscle Health, and Inflammation
Inflammation can also affect muscle health.
When inflammatory signals stay high, muscle recovery slows. Over time, this can contribute to muscle breakdown, lower strength, and reduced metabolic efficiency. That matters because muscle tissue helps manage glucose and energy use.
Adequate protein intake supports muscle preservation during periods of weight change. It helps maintain lean tissue and supports recovery, which becomes more important as people age. Preserving muscle also supports maintain a healthy weight over time.
Some structured approaches include The Smoothie Diet, often discussed in the context of organized protein intake and muscle preservation. It’s usually framed as a convenience option rather than a requirement. Reviews help readers decide if it fits their needs.
Protein alone doesn’t reduce inflammation, but it supports the body while other lifestyle changes do the work.
Sleep Quality, Recovery, and Inflammatory Balance

Sleep is one of the strongest regulators of inflammation.
Poor sleep increases inflammatory responses and disrupts hormonal recovery. When sleep is short or broken, the body produces more stress hormones, which increases inflammatory activity and makes weight gain more likely.
Sleep is also when tissue repair happens. Without enough rest, recovery slows, soreness lingers, and energy drops. This makes consistent movement harder to maintain, which feeds back into inflammation and excess fat storage.
Some people look into SleepLean when focusing on sleep quality and hormonal recovery. It’s typically discussed as supportive, not corrective. Most readers review details carefully before deciding if it fits their situation.
Improving sleep doesn’t fix everything-but it reduces one of the biggest drivers of chronic inflammation.
Frequently Asked Questions About Inflammation and Body Weight
What is chronic inflammation in simple terms?
It’s a long-lasting immune response that stays active even when there’s no injury or infection. Unlike short-term inflammation, it doesn’t turn off easily and can affect normal body functions.
Can inflammation cause weight gain?
Yes. Inflammation can change hormone signals and encourage the body to store more fat, especially when stress and poor sleep are involved.
How do stress and sleep affect inflammation?
Chronic stress and poor sleep increase inflammatory signals. Over time, this makes it harder for the body to regulate energy and appetite.
Does inflammation slow metabolism?
It can. Inflammatory activity interferes with how the body uses energy, which can reduce metabolic efficiency and recovery.
Can diet reduce inflammation-related weight gain?
Diet quality matters. Reducing processed foods and including antiinflammatory options like omega-3 fatty acids may help support balance.
Is belly fat linked to inflammation?
Yes. Fat tissue around the abdomen tends to release more inflammatory compounds than fat stored elsewhere.
Does inflammation increase with age?
It often does. Hormonal and metabolic changes after 30 make low-grade inflammation more common.
How long does it take to lower inflammation?
It varies. Some changes happen within weeks, while others take longer. Consistency matters more than speed.
Can exercise reduce chronic inflammation?
Yes. Regular, moderate activity helps reduce inflammatory markers and supports metabolic health.
Are inflammation and insulin resistance connected?
They are closely linked. Inflammation can worsen insulin resistance, which then contributes to fat storage and weight gain.
Final Verdict: Understanding Inflammation for Better Weight Management
Calories matter-but they’re not the full story.
When chronic inflammation is present, the body doesn’t respond normally to food or movement. Hormones misfire, energy drops, and fat storage becomes easier. This is why focusing only on restriction often fails.
Addressing inflammation supports balance. Better sleep, stress reduction, gentle movement, and food quality all help reduce inflammation and improve how the body manages weight. These steps don’t need to be extreme to work.
For many adults, this approach explains why weight loss feels different after 30-and why patience matters.
One Last Thought
Weight management is more than math.
Reducing inflammation supports energy, recovery, and hormonal balance. When lifestyle habits work together, progress feels steadier and more realistic.
Small, consistent choices-made daily-are what make the difference in the long run.
